In This Section:
The MD Program at the University of Toronto is one of the largest undergraduate medical education programs in Canada. We are proud to support and promote the development of future academic health leaders who will contribute to our communities and improve the health of individuals and populations through the discovery, application and communication of knowledge.
The U of T MD Program, like most North American medical schools, is four years in length. The final two years are known as the Clerkship (which involves learning while working with physicians and other health care team members in the hospital and clinic). The first two years of the program - known as Foundations - take place in laboratory, classroom, clinical, and community settings and are designed to prepare students for the workplace learning that occurs in Clerkship.
Curriculum Structure
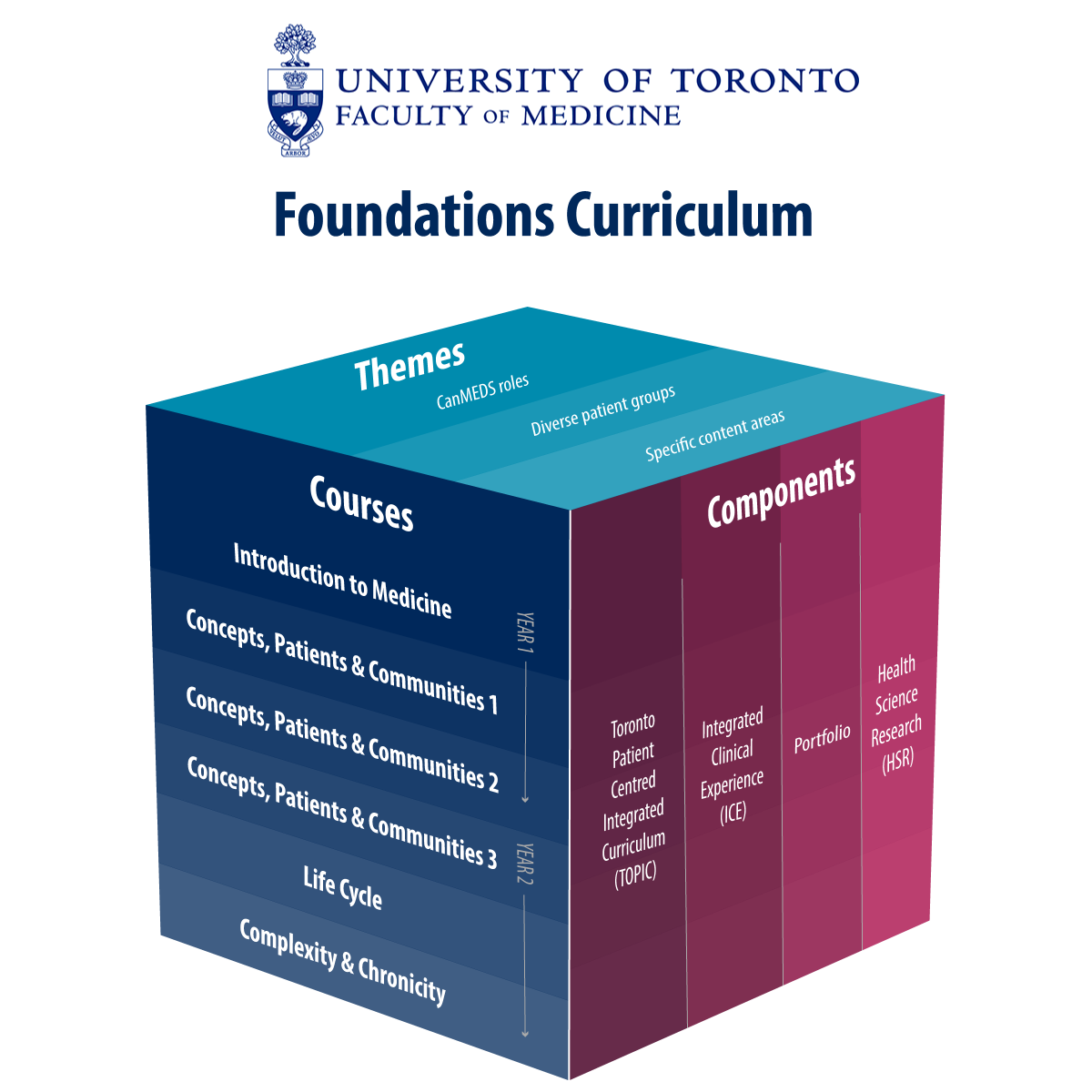 There are three major dimensions to the Foundations Curriculum: courses, components, and themes. An important feature of the Foundations Curriculum is that each week has the equivalent of a full day that is unscheduled, and available for self-study, and special activities such as clinical skill development.
There are three major dimensions to the Foundations Curriculum: courses, components, and themes. An important feature of the Foundations Curriculum is that each week has the equivalent of a full day that is unscheduled, and available for self-study, and special activities such as clinical skill development.
Courses
- Introduction to Medicine: An introduction to the basic and social sciences relevant to medicine, to cognitive science, to clinical skills and community health.
- Concepts, Patients and Communities 1: Focuses on the prevention, diagnosis and treatment of disease relevant to fundamental body systems (with a focus on introduction to pediatrics, immunity and microbiology, circulation and respiration), with integration of curricular themes.
- Concepts, Patients and Communities 2: Similar in structure to Concepts, Patients and Communities 1, this course continues a body-system approach (focusing on metabolism, gastroenterology and renal systems) with integration of curricular themes.
- Concepts, Patients and Communities 3: Similar in structure to Concepts, Patients and Communities 1 and 2, this course continues a body-system approach with integration of curricular themes. It includes exploration of body systems responsible for movement, sensation, cognition, and behaviour in humans.
- Life Cycle: An instruction on health and disease from conception, antenatal development, birth, infancy, childhood, adolescence, aging, and for patients who are dying.
- Complexity and Chronicity: A consolidation of the program with emphasis on chronic disease management, and complex problems with preparation for Clerkship.
Components
Toronto Patient-Centred Integrated Curriculum (TOPIC): In TOPIC, content is delivered through lectures, workshops, eLearning materials, anatomy labs as well as student-led and faculty-led case-based learning (CBL) sessions. In CBL, students work through a patient case in small groups of approximately 8-10 students in two sessions each week: the first one is on their own, the second is with a tutor who is a faculty member. The majority of the faculty tutors are practicing physicians based at one of the GTA teaching or community hospitals. Over the 72 weeks, the cases introduce students to all aspects of clinical medicine. Each case describes a medical problem in a patient (or occasionally a family) and offers students the opportunity to learn material in a clinically relevant way while introducing them to the scientific and humanistic foundation for the theory and practice of medicine.
Learning about the cases is supported through carefully selected eLearning materials. Each week is introduced by a half-day during which a small number of lectures provide context for the issues addressed during the week. Another half-day consists of expert-led seminars or workshops which serve to provide further context and content. Every few weeks, there is a multi-disciplinary summary lecture to help pull it all together for students.
Many of the weeks include specific instruction on the longitudinal thematic issues (described below), such as medical ethics, leadership and collaboration with other health professionals.
Integrated Clinical Experience (ICE): ICE typically occupies two half-days per week. One half-day provides students with instruction in groups of six on how to take a patient’s history and perform a physical examination (ICE: Clinical Skills).
The second half-day for ICE provides students with opportunities for early clinical exposure in a variety of settings, including doctors’ offices, hospitals, community health agencies and home care visits (ICE: Health in Community). Throughout the Foundations Curriculum, students will be able to prepare for Clerkship by spending time in clinical placement shadowing opportunities (ICE: Family Medicine Longitudinal Experience; ICE: Enriching Educational Experiences).
Portfolio: Students will spend a half-day every three to four weeks in a small group with a tutor in Portfolio. Portfolio focuses on two types of activities:
- Students will reflect on their previous experiences and their experience as first- and second-year medical students and the resulting effects on their professional development.
- Guided self-assessment: students will compile their formal assessments and the student’s reflections and develop an individualized learning plan related to these assessments to ensure students are staying on track, and receiving help where it is needed.
Health Science Research (HSR): HSR provides students with lecture, tutorial and eModule-based learning on two major topics:
- How to participate in health research projects.
- How to apply the findings of health research to patient care.
HSR also introduces students to well-known researchers working at the University of Toronto through its HSR Grand Rounds series.
Themes
Multiple themes are integrated longitudinally throughout the Foundations Curriculum and into Clerkship Overseen by faculty leads and taught by a variety of educators, the themes can be grouped into three major categories:
- Priority population groups (including Black Health, Indigenous Health, and 2-Spirit, Lesbian, Gay, Bisexual, Transgender, Queer, Intersex and Asexual+ Health)
- CanMEDS roles (e.g. Leader)
- Specific content areas (Public Health, Interprofessional Education, Quality, Safety & Value)
In addition to providing leadership for curriculum development and delivery relevant to their themes, the Black Health and Indigenous Health theme leads play an active role in Temerty Medicine’s efforts to diversify its student body.
For more on the MD Program's curricular themes: http://md.calendar.utoronto.ca/curricular-themes
Educational Learning Modalities
The students’ weekly teaching and learning experience will occur using a variety of learning modalities that are selected based on the desired learning outcomes and the integrated blended learning teaching model that is used in the MD Program Foundations Curriculum. Modalities that are used to meet the learning outcomes include: (a) Independent Learning; (b) Large Group Lectures; (c) Small Group Learning/Discussions (d) Anatomy Labs; and (e) Experiential Learning.
Each of these learning modalities is described below with examples on how it is used in the MD Program Foundations Curriculum.
Independent Learning
Each week students are provided learning content that they are expected to learn on their own. This material has been specifically selected or designed to provide foundations content required to effectively engage in subsequent learning tasks during the week.
Pre-week preparation (PWP)
- These are online foundational resources (e.g., readings, videos, e-learning Modules, etc.) that support basic learning objectives of the week.
- Students are expected to study independently these materials and understand the content prior to the start of the weekly lectures.
Self-learning modules
- Certain learning outcomes that are not covered by one of the other face-to-face educational learning modalities described in this document can be addressed by students independently through: (a) preselected or predesigned readings; (b) e-learning Modules; (c) education videos; (d) or practice exercises with answers.
- Students are expected to study these materials independently during the week in preparation for small group discussions and mastery exercises.
Large Group Lectures
Each week, some teaching occurs in the form of large group lectures. Large group teaching may occur in-person (with videoconferencing to other sites when required), or, entirely virtually. Some, but not all, of these lectures are recorded for future viewing.
Foundational lectures for TOPIC
- There are live lectures that are scheduled on the first day of each content week. These lectures may serve several purposes:
- To build on material covered in the pre-week preparation
- To serve as a broad introduction to material that will be covered in greater depth in the Case-based learning (CBL) and self-learning modules
- To provide an opportunity to teach concepts best conveyed in a lecture format
These lectures are designed to be engaging and incorporate various active learning strategies (e.g. use of audience response system, questioning, small group dialogues, using patient or clinician panel) instead of the traditional didactic style. Lecturers may quiz the class on the PWP materials to identify learning gaps for further discussion during lectures. This is a form of “flipped-classroom” – the students are expected to be prepared by completing the pre-week learning (see Independent Learning description) before coming to lectures for a more engaging active learning experience.
- There are live lectures that are scheduled on the first day of each content week. These lectures may serve several purposes:
Component and Theme Lectures
- These sessions are led by faculty and/or content experts, including non-physicians. They will teach and interact with students on content and skills relevant to a particular component/ theme (e.g., ethics, leadership).
Integrated and application lectures (ISAL)
- These lectures occur at the end of every sub-section of each course and provides an opportunity for faculty to summarize key concepts, to reinforce learning points, and to teach about any challenging/difficult concepts encountered by students (e.g., during CBL or weekly feedback quizzes). Some of this review will be directed by students’ questions that have arisen throughout the subsection. There is also an opportunity for students to ask questions during the ISAL.
- Sample multiple-choice questions and/or clinical cases are often used during ISAL to demonstrate the application of concepts. Patients may also be invited to discuss their lived experiences, which will help to bring the conditions taught to life and to provide students with a more comprehensive understanding of both the medical and psychosocial aspects of such conditions.
- Attendance is mandatory when patients are present. From time to time, additional material (e.g., previously not discussed case examples or slides) may be introduced in order to reinforce or clarify concepts previously taught. This material will not be assessed per se, but the learning objectives relating to these materials will be highlighted by the faculty.
Small Group Learning
To support guided discovery learning a significant proportion of teaching and learning opportunities occur in small groups guided by a faculty member. Small groups may be run as tutorials, workshops, or seminars.
Tutorials
Tutorials include the following: (a) Case-based Learning (CBL) tutorials; (b) ICE: Health in the Community (HC) tutorials; (c) ICE: Clinical Skills tutorials; (d) Portfolio Tutorials; and (e) Health Sciences Research (HSR) tutorials.
CBL Tutorials
- CBL tutorials focus learning around a weekly patient case that is presented as a virtual patient in an online module. Student learning occurs in a group of approximately 8-10 students who go each week through the CBL module in two face-to-face small group sessions. The first CBL tutorial is run by students on their own (student-led face-to face discussion) and the second is guided by a CBL tutor (faculty-led). Within each case, there are approximately 10-15 embedded questions that represent typical questions that a preceptor could ask during bed-side clerkship teaching and that require student learning that aligns with the weekly learning outcomes. Some of these assignment questions are to be responded to together by the group (group questions) during their first CBL session and the rest are to be prepared by each student on his or her own (independent study questions) prior to the second CBL session.
- CBL cases include “what if scenarios” - questions posed by CBL tutors during faculty-led CBL. These are new questions students have not seen before. The goal of this activity is to expose students to meaningful contextual variation, as in, looking at the concepts in the CBL from a different context or angle.
ICE: Health in Community Tutorials
- These tutorials are led by a team of two academy-based tutors including one physician and an allied health professional. Tutorial groups contain approximately 6-8 students. The ICE: HC tutorials provide an opportunity for small group discussion and reflection. Tutors will guide students through discussion of cases, videos, podcasts and articles focused on topics related to social determinants of health, health promotion, disease prevention and public health and population health. In addition, the tutorials also support student engagement with CEEs (Community Engaged Experiences) in year 2.
ICE: Clinical Skills Tutorials
- During the Clinical Skills Tutorials, students learn the clinical skills of interviewing, history-taking, physical examination, and communication, as well as how to interpret the data in a diagnostic formulation, document and present it. Instruction takes place at the academies in small groups facilitated by one clinical skills tutor (or occasionally two tutors) per group.
- The tutors are responsible for teaching the basic clinical skills to the students, who often initially practice the skills on each other or sometimes on “standardized patients” and subsequently on real patients. The students are assigned particular tasks in each tutorial, and the tutors are responsible for observing the students’ performance and correcting any deficits.
- Students receive feedback from their tutors throughout the courses, based on both direct observation and submitted written work.
Portfolio Tutorials
- Portfolio sessions allow students to reflect on and discuss their experiences as medical students and to develop their identity as future physicians.
- The tutorials are facilitated by Senior Academy Scholars and Junior Academic Scholars.
- Twice a year students meet with their Senior Academy Scholars for a progress review and develop their own individualized learning plan
HSR Tutorials
- There are several HSR tutorials in year 2 which occur in small groups guided by an HSR tutor.
- Through discussion, opportunities to struggle and to apply research principles, students learn how to become effective consumers of research and to contribute to improving the health of patients and populations.
- When possible, examples are used in HSR tutorials of articles that align with content discussed in CBL cases of the week.
Workshops
Skill-based workshops
- The focus of these workshops is to learn and practice a specific clinical skill (e.g., ECG workshops) under the guidance of a faculty expert.
Clinical Decision Making Workshop
- The purpose is to provide active learning opportunities for students to practice clinical decision making related to a variety of clinical situations.
Seminars
- Seminars occur in small to medium-sized groups and are held either centrally at the St. George and Mississauga campuses or at the academy sites.
- Types of seminars may include theme related topics such as: Ethics; Interprofessional Education (IPE); Leader; or Pharmacology.
- Seminars are led by faculty and/or content experts, including non-physicians.
MAPS
- MAPS is an integrated curriculum including medical imaging, anatomy, pathology and surgery which occurs throughout year 1 and 2 and is integrated into the TOPIC curriculum.
- Teaching sessions include medical imaging, anatomy, and pathology lectures focusing on core curriculum and integrated multidisciplinary rounds.
- Core anatomy is taught through lectures, dissection labs, and small group activities.
- Medical imaging and pathology teaching is also supported through small group case-based tutor-led sessions.
Experiential Learning Opportunities
Throughout Integrated Clinical Experience (ICE), there will be opportunities for experiential learning. This will include interactions with standardized patients, real patients, and role-play (simulation of a health care provider encounter). Experiential learning will allow students to develop skills (i.e., communication), receive feedback in a safe environment, overcome anxiety related to speaking in front of others, inform future career decisions, enhance students’ learning of clinical medicine, and gain insight into the patient experience.
The different types of experiential learning opportunities that have been integrated in the curriculum include: (a) Standardized Patient Encounters in ICE: Clinical skills; (b) Real patient encounters in ICE: Clinical Skills; (c) Enriched Education Experiences (EEEs); and (d) Community Engaged Experiences (CEEs) in ICE: HC.